The Importance of Reconciliation in Medical Billing
It’s not just about counting coins; it’s about monetizing accuracy to carve a niche in the bustling ecosystem of healthcare innovation. Through these strategies, healthcare organizations can achieve a level of financial clarity that not only stabilizes their operations but also propels them towards sustainable growth. The end result is a healthcare system that is robust, reliable, and ready to adapt to the ever-changing landscape of healthcare needs and economic demands. In addition to providing increased transparency and payment integrity, our reference-based pricing solutions and clean claim reviews can help you save up to 40% on your healthcare spend and reveal the true value of quality healthcare. A leading cost-containment method, it uses aggregate prices for services to negotiate more reasonable payments.
Why Healthcare Reconciliation Matters?
This process is essential for ensuring the financial integrity of healthcare institutions, tracking payments, detecting discrepancies, and minimizing errors. Cash reconciliation software and services contribute to the efficient management of revenue and financial records within healthcare organizations. An integral part of this process is payment reconciliation, which involves verifying that the payments online bookkeeping received match the billed services. This step is essential for identifying discrepancies such as pending receivables, underpayments or denials and resolving them efficiently. Effective payment reconciliation helps keep accurate financial records and makes sure healthcare providers are paid correctly. Cash reconciliation software and services are vital components of healthcare revenue cycle management.

Navigating the Payment Reconciliation Process
- This metamorphosis is not just theoretical; it is evidenced by real-world triumphs that have redefined the financial landscapes of healthcare institutions.
- This complexity is not just a byproduct of the system’s vastness but also of the nuanced interplay between these entities, each with its own set of expectations and obligations.
- In the realm of healthcare finance, the transformation from disarray to precision in payment reconciliation stands as a testament to strategic ingenuity and operational excellence.
- This can be a lengthy and frustrating process, but it is essential to ensure that providers are fairly compensated for their services.
Seeing firsthand how unsuspecting patients are frequently confused by an overly complex system they don’t understand led Burns to become an insurance agent and health care consultant, now helping people understand the medical system. Understanding the budget reconciliation process, including the importance of the budget resolution and its potential rapid consideration in the new year, is therefore of key importance, especially in light of potential threats to Medicaid. Through these lenses, payment reconciliation transcends its traditional role, becoming a catalyst for growth and sustainability in the competitive healthcare market.

Finance Automation Trends and Statistics for 2025
Providers, payers, and policymakers must adapt to ensure sustainable healthcare delivery while prioritizing patient well-being. Leo John is a finance strategist and IT professional at Bookkeeping for Chiropractors MHRCM and is passionate about revolutionizing revenue cycle management (RCM). Medical coding and billing is a sensitive and integral segment of healthcare service provision. Patients feel cheated when they’re billed incorrectly, and this could cut short long-established professional relationships. One of these challenges stems from complicated insurance policies with different rules and requirements. Despite the enormous amounts of money the United States spends on healthcare, prices continue to rise.
- Collecting patient payments and recording them accurately in financial systems should not contribute to that stress.
- Through these lenses, payment reconciliation transcends its traditional role, becoming a catalyst for growth and sustainability in the competitive healthcare market.
- This comprehensive approach ensures that healthcare providers are paid fully and promptly for the services they deliver.
- Reconciliation helps detect these instances, ensuring providers return any excess funds to maintain accurate financial records and comply with regulations.
- The main procedural advantage is that reconciliation bills are limited to 20 hours of debate and not subject to filibuster; therefore, reconciliation bills can move forward and pass with a simple majority vote.
For financial management, compliance, analysis, and decision making, revenue reporting is a critical step. This is where providers generate statements and financial reports that summarize revenues from provided services to patients. Revenue reconciliation is the process of reviewing claims, payments, and adjustments to ensure that payments are recorded properly within the provider’s own systems and paid accordingly by patients. If you want to automate this process, contact us today to schedule a meeting and learn more about our billing solutions. With this, providers can identify any shortfalls and take action to recover the missing amounts.
Top 10 Automation Challenges for CFOs
The Mayor’s Office for Economic Opportunity uses evidence and innovation to reduce poverty and increase equity. It advances research, data and design in the City’s program and policy development, service delivery, and budget decisions. She earned her nursing degree in 1990 from Jacksonville State University, obtained her insurance billing and coding certification in 1995, and holds a health and life insurance license in Alabama, Georgia, Iowa, Mississippi, and Tennessee. Burns is Affordable Care Act (ACA)-certified for health insurance and other ancillary, life, and annuity products. The sweeping health section of the continuing resolution text is now circulating, and a copy obtained by Axios shows it includes major provisions on PBMs, hospital costs, telehealth and other health extenders.
Partner with us for ComprehensiveIT Services & Solutions
In order to have documentation to compare, you must have documentation in hand to review. When working across offices and locations, paper-based trails are going to cause obvious delays and hardships. Freed assembled a project design and steering committee, which included representatives from the client’s Finance, Information Systems (IS) and Patient Financial Service (PFS) departments. With Freed’s oversight, this group collaboratively identified multiple improvement opportunities in payment processing workflows. Learn how the power of social care and medical care partnerships are improving health equity. Cost of Goods Sold (COGS) and Gross Margin are two essential metrics that businesses use to analyze…
Healthcare payment reconciliation: From Chaos to Clarity: Business Lessons from Healthcare Payment Reconciliation
- Detailed documentation of current processes is essential to identify key areas for automation.
- Providers, payers, and policymakers must adapt to ensure sustainable healthcare delivery while prioritizing patient well-being.
- Visit BPO for Healthcare Providers to learn how you can use RPA in reshaping your healthcare finance.
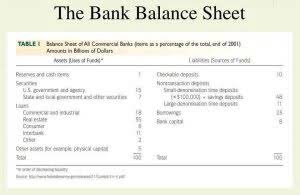
- By examining these components, one gains a deeper understanding of the financial underpinnings that support the delivery of healthcare services.
- Managing and reconciling this data accurately can be overwhelming and time-consuming, increasing the risk of errors.
- They provide a comprehensive view of financial and operational data, making the reconciliation process more seamless and efficient.
With a consistent medical billing reconciliation process, providers and insurance companies can maintain solid working relationships in an effort to provide value to the patients who need healthcare. Navigating these regulations requires a robust compliance program that includes employee training, regular audits, and a culture of integrity. For example, a hospital might implement software that automatically flags what is payment reconciliation potential AKS violations, such as a pattern of referrals to a particular service provider. By staying vigilant and proactive, healthcare organizations can turn the chaos of payment reconciliation into clarity, ensuring that they operate within the law while providing the best possible care to their patients. Compliance is not just about avoiding penalties; it’s about fostering trust and safety in healthcare transactions. These enhancements have allowed the healthcare system to enjoy increased financial accuracy and proficiency, and have served as a catalyst to implement additional operational improvements.
MHRCM Insights to Streamline Revenue Cycle Management and Enhance Efficiency
But whichever system is used, the accuracy and efficient posting by your billing team comes first. The problem providers face is a Byzantine payment process—a complex and unwieldy method of managing healthcare payments created by decades of varying market forces. As a healthcare finance professional, you are all too aware of the importance and need to have an accurate and timely medical billing reconciliation process. When it comes to medical billing reconciliation, the process is both inherently unique and naturally complex due to regulations, policies, and the vast array of services provided. The claims reconciliation process can be complex and time-consuming, but it is essential to ensure that patients receive the correct care and reimbursement from insurance companies. Reconciliation ensures healthcare providers get timely and accurate reimbursements, which helps keep their revenue stable.




